Value Add Intermediaries in FHIR®
How FHIR standards could support responsible exchange of enhanced data
How FHIR standards could support responsible exchange of enhanced data
At Availity, we are very excited about the continued adoption of Fast Healthcare Interoperability Resources (FHIR®) within the healthcare industry. However, history has shown that healthcare data format standards are only one part of the solution. FHIR alone cannot address the challenges found in the numerous ways that healthcare data is encoded and often hidden in clinical notes, images, and other narrative reports. Interoperability is critical to the modernization of healthcare and we, at Availity, want to see FHIR succeed so that we can all reap the benefits.

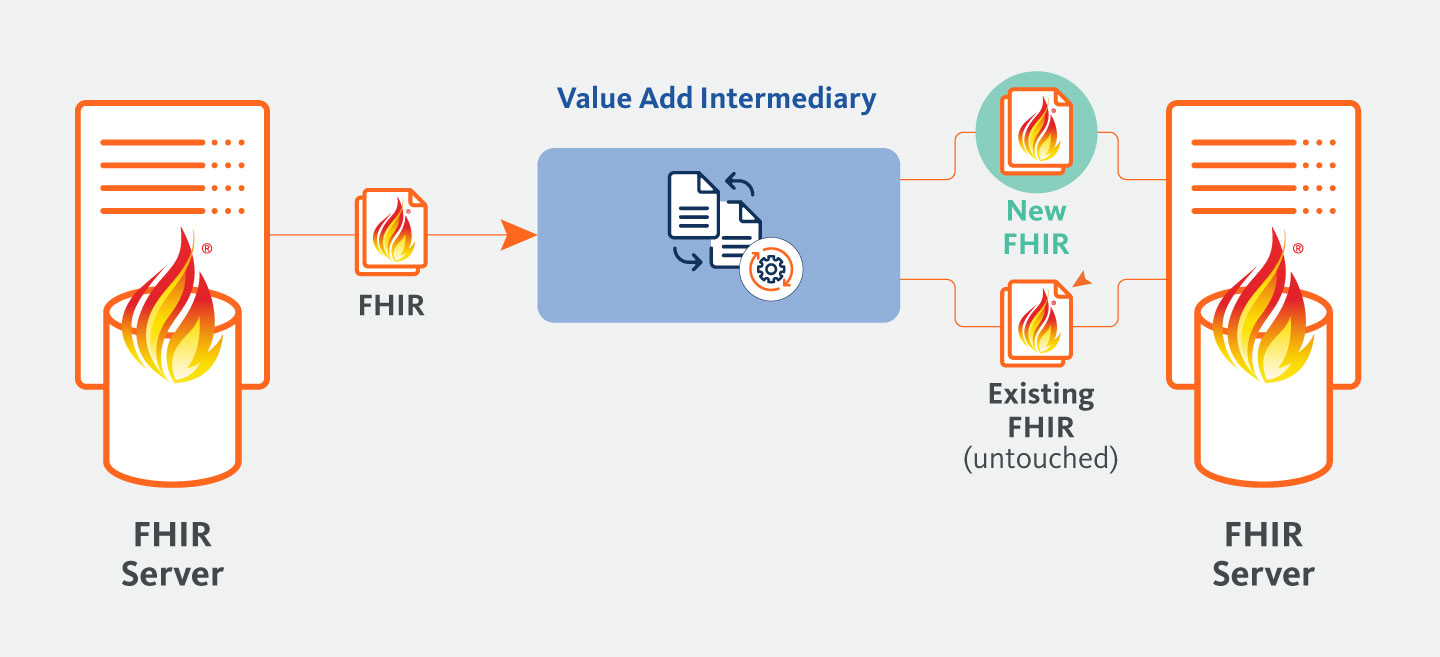
If FHIR is going to succeed, it will be critical to introduce Value Add Intermediaries (VAI). VAI are organizations or platforms that operate between healthcare stakeholders, such as patients, healthcare providers, insurers, and regulators, to facilitate value-added services and improve outcomes. These intermediaries may leverage technology, data analytics, and other tools to drive innovation, efficiency, and collaboration across the healthcare ecosystem. VAIs can help improve the quality of data, expose data hidden in narrative form, identify missing data, and many other functionalities we can’t envision yet.
VAIs have the potential to make the dream of interoperability a reality. By providing services, like data quality improvement, VAIs can enhance multisource and multi-format data in ways that make it more understandable and actionable. Beyond that, VAIs can revolutionize the practice of medicine by unlocking data from narrative text and enriching it with predictive analytics. Finally, they can take quantitative data and translate it into qualitative stories that are understandable and actionable by patients, providers, and loved ones.
However, this data must be represented responsibly and used only for appropriate uses that are tolerant of the inherent risks. The FHIR standard needs to evolve to allow the capture of this data, along with the original data.
enhanced use of provenance
new resource types
effective use of the
meta tag
However, the purpose of this paper is not to propose any particular change but instead raise awareness of the powerful possibilities that VAIs bring to the table.

Health data is extremely fragmented. Healthcare is, arguably, the second oldest profession in the world. It should be no surprise that documentation in healthcare is so varied. After all, for a long time this documentation only served to help the provider, as one patient only had one doctor. Even as the idea of medical institutions grew and doctors formed practices where more than one doctor might see a patient, these were islands to themselves. However, today’s world is far more mobile and complex. Patients often see providers in other parts of the country or even other parts of the world. On average, patients see two primary care providers and seven specialists from four practices each year.1 This has made interoperability extremely important to the continuity of care.
Problems arise when we try to use data from one institution in another, because each institution has its own practices and procedures for recording healthcare data. This stems both from divergent histories and from licensing, specialty, and regulatory variations. One institution may have licensed one code system, while the institution down the street licensed another. Additionally, one code system may support cardiology better than orthopedics, or the like. These variations make it impossible to exchange the data in a meaningful way.
While many thought that electronic health records (EHR) systems would solve this problem, the reality was that EHRs were entering a fairly entrenched world that was understandably resistant to change. In many cases, the EHR had to adapt to the realities on the ground, instead of imposing conformity. EHRs are a massive step forward, but they do not answer all the problems of interoperability.
“On average, patients see two primary care providers and seven specialists from four practices each year.1 This has made interoperability extremely important to the continuity of care.”
New standards, like FHIR, certainly help. FHIR provides a consistent format for the data, merging the variations of shapes into a single, recognizable shape. However, this only answers for the form of the data. It does not help with the contents within. To follow the analogy: FHIR may specify that all data of a certain type must be represented in a circle, but, for the most part, it doesn’t say what the difference between a red and green circle is. This means that FHIR provides a standard format for organizing and exchanging data for a specific type, but it doesn’t dictate the interpretation or significance of different variations or aspects of that data.
Additionally, a lot of healthcare data is trapped in narrative notes, reports, and images. Not to mention the quantity of data that is outright missing for any number of reasons, from patients not disclosing certain information to errors in data entry and inadequate data collection procedures. New technologies are springing up every day in the fields of Natural Language Processing (NLP) and Artificial Intelligence (AI), that can help unlock that data. They can also enrich the data, with analysis and predictions that can greatly aid doctors and patients in making more informed decisions. However, the results from these systems are probabilistic in nature and great care must be taken to use them appropriately.
“New technologies are springing up every day in the fields of Natural Language
Processing (NLP) and Artificial Intelligence (AI), that can help unlock that data. They can also enrich the data, with analysis and predictions that can greatly aid doctors and patients in making more informed decisions.”
AI systems can be seen as one type of a larger classification of VAI. VAIs sit between producers and consumers of data and work to make the data more understandable and actionable. Below are some scenarios that VAIs address:
VAIs can range from highly deterministic, for use in regulated environments,
to more probabilistic systems, which need to be handled with more care.
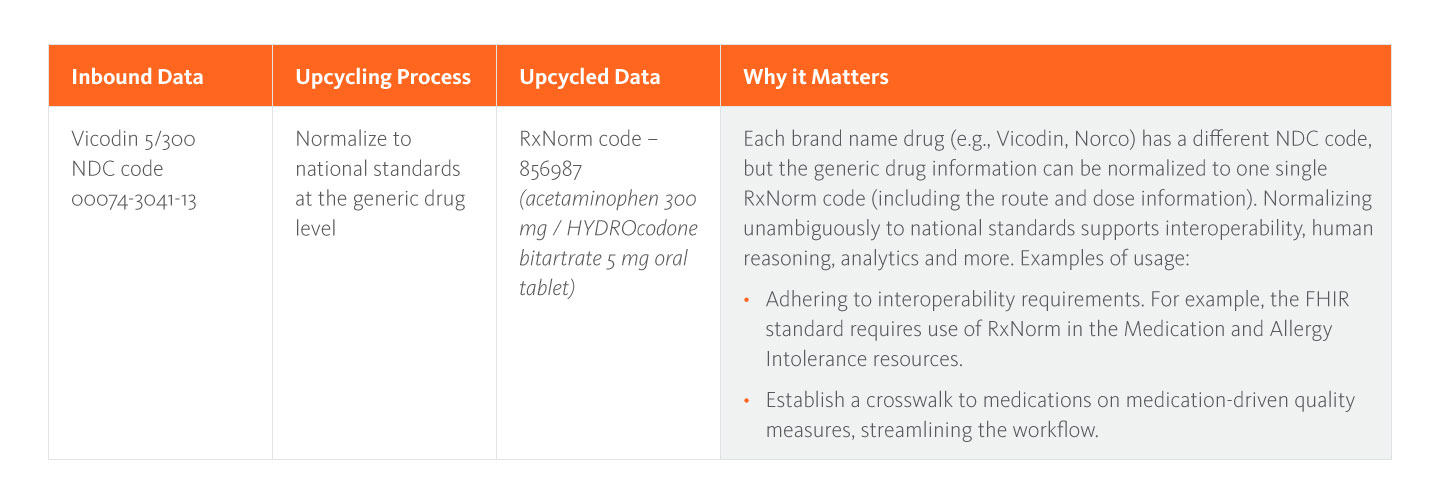
There are often very deterministic ways to move data from one standard to another. This includes code mapping, where the system understands that code A in system 1 maps to code B in system 2. However, even more advanced techniques can be applied, such as using key words in descriptions to match uncoded values to codes in a code system. At Availity, we call this process Upcycling Data™, which, in addition to this normalization, includes enriching, reorganizing, and deduplicating data via our API-based Availity Fusion™ technology engine.
In cases where data is coming in from an EHR, lab system, or other electronic system, Upcycling Data can often add tremendous value to the data. It can determine that while source A has a red circle and source B has a green circle, in reality both are blue circles in the national standard for how circles are understood. Further, it can decorate the blue circle with information, tell where the blue circle should appear in the record, and determine if two blue circles are the same. All of this results in data that is far easier to leverage in the consuming system.
To put it into perspective, Upcycling Data can help to ensure that the clinical data being exchanged through a Health Information Exchange (HIE) is consistent, complete, and accurate, regardless of where it was sourced. For example, a patient’s medication record may be represented differently in the EHR system used by their primary care physician and their specialist, resulting in discrepancies or inconsistencies in the data. By Upcycling Data, the HIE can identify and reconcile any differences, ensuring that the data is represented consistently and accurately across both systems. The upcycled data can also be enriched with additional metadata, such as the source of the data, the date of the medication order, and the dosage instructions, making it more valuable for clinical decision-making.
AI has been exploding in the last few years. While it is laughable to suggest that AI will replace doctors, it does have tremendous potential to revolutionize the practice of medicine. As my colleague, Paulo Pinho, M.D., Vice President, and Medical Director of Innovation at Availity, says, “The black bags of physicians today contain stethoscopes, reflex hammers, and ophthalmoscopes. The black bags of the future will need to contain AI tools in order to meet the demands of an evolving medical body of knowledge.”
However, the power of AI is not limited to what it will do for doctors. In the increasingly complicated world of medicine, it is critical that patients and their loved ones become highly involved in their healthcare. Most of these people are not medical professionals and need help understanding the nuanced data available in health records. AI can take this quantitative data and represent it in a qualitative narrative to help non-medical professionals make good decisions.
Nevertheless, AI is far from foolproof and the majority of it is probabilistic in nature. Great care must be taken to use this data responsibly. Different uses of this data will have different tolerances for the inherent risk of this data being incorrect. For example, population health analytics across large populations often have a high-risk tolerance for use of this data. In a large population, the added data can erase biases, regional inconsistencies, and so on, while the inaccuracies are reduced due to the sheer volume of data. On the other hand, highly regulated programs, like HEDIS® and Risk Adjustment Factor (RAF), may have far less risk tolerance for AI data. Below we will discuss in detail “responsibly” representing data.
“While we can’t predict what these VAIs will do and how they will do it, we can
prepare for their arrival. By building into our standards and interoperability flows the room for VAIs, we leave the door open for others to be inserted with far less pain.”
If there is one thing that can be certain in medicine and technology, it is that we have no idea where the future will take us. Above we outlined two scenarios for VAI, but there is no doubt that there will be others. While we can’t predict what these VAIs will do and how they will do it, we can prepare for their arrival. By building into our standards and interoperability flows the room for VAIs, we leave the door open for others to be inserted with far less pain.
For example, if we adopt some of the suggestions around the use of the FHIR meta tag below, we make it possible for future VAIs to also identify resources they have generated or touched.
While future proofing is often a foolhardy undertaking, it still makes sense to leave hooks in our standards to support the future. The difference lies in creating something that may not have present-day applications, as opposed to designing a useful structure for today with flexibility to adapt for future needs. VAIs exist today and the need for them will only grow. Therefore, by supporting VAIs today in an open way, we can lay a solid foundation for the future.
VAIs provide tremendous power, but it is virtually impossible for any VAI to be 100% accurate because healthcare is a complex and rapidly evolving field, and there are numerous factors that impact the accuracy and effectiveness of VAIs. Instead of rejecting VAIs entirely, we need to approach them responsibly, depending on the risk tolerance of the use case. For example, a care manager at a health plan who is looking to make sure their members get the right preventative care could benefit from a VAI that can help identify which patients are most in need. However, it would be irresponsible to use that same VAI to replace a triage nurse in an emergency room.
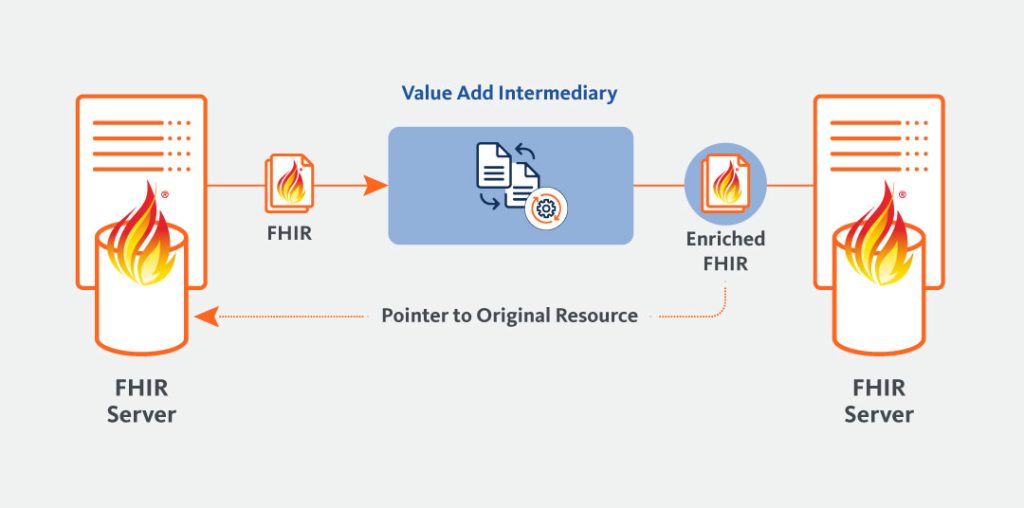
The key to responsible representation is first clearly labeling data that has been generated or touched by a VAI. Then, we must also make it clear what sort of VAI was involved and what confidence the VAI has in its inference. Further, we must make it easy to retrieve the data in its original form. In some cases, this means separating the VAI data into distinct resource types, while others may simply provide ways of getting to the original data or may place the VAI data beside the original values.
Let’s explore how a few of these might play out.
At Availity, we have already proposed a way that the Provenance resource type, a single activity that identifies a set of resources (target) generated by the activity, could be utilized to solve the problem of providing access to original resources.
The FHIR standard already allows every resource to be associated with a Provenance resource. The purpose of the Provenance resource is to detail the lineage of the resource. It can also provide links to additional resources. The essence of this solution is to store a copy of the untouched resource before it goes through the VAI. The VAI then modifies the resource and sends it on with a Provenance resource that links back to the untouched copy. Downstream systems can then decide whether or not to fetch the untouched resource or not.
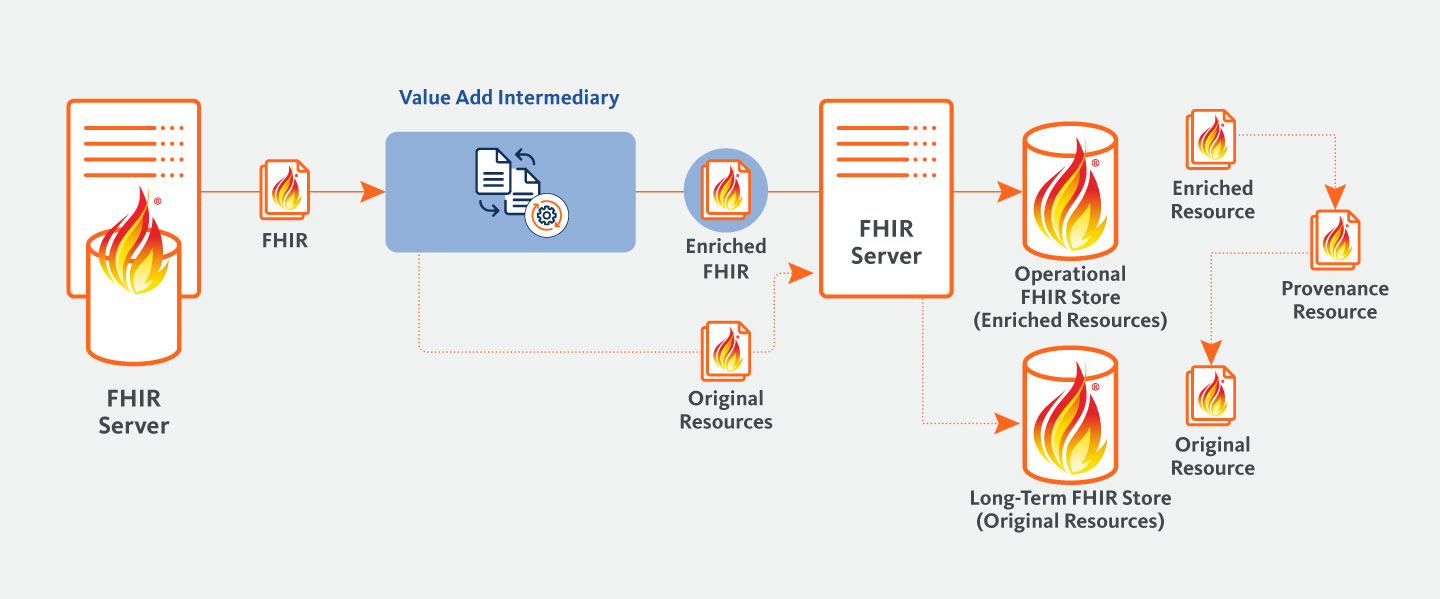
There are two main advantages to this solution over placing the VAI data alongside the original data in the resource:
When looking at the outputs of many NLP and AI systems, it is clear that they are ripe for standardization. At Availity, we published a paper called “FHIR-Enabled AI: A Proposal for Standards for Output from AI” that outlines what that standardization could look like.
This paper suggests that we keep the results of certain VAIs in new FHIR resource types. There are a number of reasons for this, but of particular interest here is the fact that it clearly separates the data. For example, some have suggested that NLP/AI results can be captured in Observation resources. However, this means that a downstream system can’t know the difference between an Observation that is from a certified record vs. one that is from an NLP. It also muddies the water, with many Observation resources that are actually other resource types, like Conditions, but because they were found by NLP they are trapped within Observations. If we follow this liberal definition, we might as well make all data Observations, because it is all from some form of observing the patient. In cases where the Observation, Condition, or other resource, is useful, a standard mapping is proposed from the new resource type to existing resource types.
While the Provenance resource is very powerful, the FHIR specification has no requirement that downstream systems request the Provenance for any resource. This creates a problem if the Provenance is the only place where the fact that a VAI was involved is indicated. In “FHIR-Enabled AI: A Proposal for Standards for Output from AI” we introduced standards for NLP/AI outputs, we discussed using the meta tag to solve this.
The FHIR specification allows for every resource to have a meta tag that provides meta-data about the resource. This tag, if present, is transmitted with the resource. The paper calls for adding optional fields to the meta tag that could be used to indicate that a resource was created or touched by a VAI. These fields would be a small subset of what could be gained from the Provenance. While downstream systems might still ignore the meta tag, they will have at least received the information.
If VAIs are going to take their place as a standard part of our data pipelines, then we need the industry to take action.
Organizations like the Centers for Medicare & Medicaid Services (CMS) have a huge impact on how healthcare data is exchanged. Both because of regulations like the Patient Access Final Rule and because of the way they consume data, like HEDIS and RAF. Some regulatory bodies are resistant to VAIs because they are concerned that any intermediate process might “game the system” by changing the data in a way that makes the results (quality scores for example) better. However, regulatory bodies who are resistant to VAIs may miss out on valuable data because of the fragmentation discussed above. As technology progresses, the amount of value being missed will only increase. Instead of ignoring VAIs, regulatory bodies should embrace them, but do so responsibly, by leveraging some of the ideas presented here. For example, regulations may allow for the use of data from VAIs as long as it is properly tagged, and its importance is weighted appropriately.
“In order to avoid the mistakes of the past, it is important to get ahead of these technologies and provide ways to capture this data in standards so that it is possible to leverage it in the future. If not, we will see a wild west of data formats that make for an interoperability nightmare.”
Everyone involved in healthcare needs to demand better access to higher quality data and the ability to understand that data. No one should be satisfied with simply passing on bad data because that is how it came to them. All the players need to understand the value that VAIs bring, along with the risks. They need to think hard about their use cases and when the value of VAI data outweighs the risk. Then they need to demand that VAIs be allowed to responsibly drive better outcomes and contain costs.
Whether you are a healthcare industry leader, provider, or healthcare consumer, you have a role to play. It’s crucial to understand the value vs. risk of VAIs and recognize the limitations of the data you are currently using today. You should also think about the data you’re missing that could be helpful. Then you need to raise your voice and talk to providers, health plans, standards bodies, and regulatory bodies and demand the highest quality data be made available to you when you need it, in a responsible way. There are many players in the world of healthcare, but in the end, you are the one primarily responsible for your well-being. Take steps to make sure you have the high-quality, understandable, and actionable data you need to take on that responsibility.
Don’t Wait: With up to 5 billion exchanges of digital health information annually, the tide of clinical data keeps rising. Start upcycling your data into a clean, concentrated, usable force today.