Operational ROI
How health plans use Availity’s automated, scalable technology to maximize value from clinical data investments and avoid significant operational cost
How health plans use Availity’s automated, scalable technology to maximize value from clinical data investments and avoid significant operational cost
Today, health-related data’s ever-growing footprint, generated by sources like electronic health records (EHRs), personal fitness applications, lab results, and home genome test kits, is rapidly outpacing that of other industries such as finance and manufacturing.1 In fact, data scientists estimate that around 30% of the world’s data volume comes from the healthcare industry.2
Clinical data has historically resided in silos, but increasingly those silos are breaking down. Health plans, specifically, invest significant dollars in the acquisition of clinical data sources, but quickly find that this data is challenging to use at scale in its raw form.

Once acquired, clinical data must be normalized and optimized for successful deployment across downstream applications and to maximize return on investment (ROI). Resource-heavy manual processes that are traditionally available to make clinical data organized and interoperable are costly, inefficient, and inhibiting. As such, health plans are looking to invest in specialized vendors that drive efficiencies through reliable automation and demonstrated scalability at the enterprise level.
The Availity Fusion™ API-based technology automates clinical data integration, normalization, and enrichment in real-time and at scale via a comprehensive five-step process known as Upcycling Data.™ Lucy Parente, Director of Strategy, and Chun Li, Ph.D., Vice President of Informatics at Availity, partnered with a large national health plan to develop an Operational Cost Avoidance Model to quantify the return on investment using Availity Fusion in place of manual methods.
The Availity Clinical Solution’s informatics team provided data on the time and resources needed for Upcycling Data based on their experience of nearly a decade in this field, as well as the number of terms per clinical domain in the provided dataset. The health plan partner shared their extensive experience by contributing the document count, member count, and number of resources currently involved in data quality activities.
Investing in Availity Fusion can be a cost-effective way to enhance data quality and interoperability. By doing so, actionable clinical data becomes an asset that is available more quickly and sustainably.
Despite investing millions of dollars in clinical data acquisition, the health plan acknowledged that the variability and volume of systemic clinical data would make it challenging to achieve the promised return on investment in a cost effective manner.
cost to a mid-sized health plan for manual resources to perform data improvement functions
potential cost avoidance with a large national health plan
Availity’s ability to optimize clinical data 17,800x faster than manual resources

Once clinical data is acquired, the journey to deploy and capitalize on this investment has just begun. Clinical data in its raw form is incredibly challenging to use. Availity found that up to 50% of data contained within standard clinical sources is incomplete, non-standard, and non-interoperable.3 The inherent variation in source documentation and accuracy, plethora of custom and standard terminologies, and fragmented storage of data across the healthcare system all contribute to clinical data’s complexity. To combat these challenges, health plans must make a strategic investment in data quality improvement.
Research conducted by Gartner®, a technological research and consulting firm, indicates that for clinical data to be effectively used in processes such as care coordination and utilization management, it needs to be both syntactically and semantically interoperable, conforming to both structure and content.4 Due to the complexity of this process, it is highly recommended that organizations seek expert assistance from a vendor to normalize clinical data.
From semantic normalization to flexible enterprise data integration, it is critical to invest in data quality improvement to maximize ROI and realize the value of clinical data across enterprise functions. Without this investment, health plans risk poor business performance, including inaccurate risk adjustment and quality measure compliance, burdened staff who cannot operate at the top of their license, inability to respond to government mandates, inhibited growth and innovation, and, most importantly, poor member health outcomes and care experiences.
“Research conducted by Gartner® indicates that for clinical data to be effectively used in processes such as care coordination and utilization management, it needs to be both syntactically and semantically interoperable,
conforming to both structure and content.”
This investment takes two major forms for a health plan:
When building out this function using internal resources, there are significant barriers to success to consider. One of these obstacles is the prevalence of manual processes, which can be:
In a study performed by Availity, it was found that it may take up to four hours for a data analyst to improve the interoperability and usability of a single Continuity of Care Document (CCD) manually.5 For a mid-sized health plan with ~100,000 members and an average 3:1 CCDs per member, the time and effort to improve the data quality would need to scale significantly. Tasks required include data ingestion, loading, parsing, normalization, enrichment, reconciliation, and de-duplication.
Additionally, terminology mappings and reference sets must be maintained and continuously updated to ensure accuracy as new sources are onboarded and national and industry standards are updated. This inefficiency prevents growth and scalability of business operations, while also hindering daily processes with errors and inconsistencies that yield poor results. Further, most healthcare data scientists and related staff, including clinical staff, report burnout and mental health issues due to unexpected workloads and burnout. As a result of tedious documentation and data quality improvement tasks, a recent study showed that only ~22% of data engineers’ time is spent on innovation.6
Significant
Delays & Cost
Poor Business Outcomes
Resource Burnout
Inability to Innovate
“As a result of tedious documentation and data quality improvement tasks, a recent study showed that only ~22% of data engineers’ time is spent on innovation.”
Choosing to apply automated, scalable technology allows organizations to accelerate the deployment of clinical data to drive business transformation, reallocate existing resources, and optimize financial and clinical outcomes. Health plans are taking advantage of this interoperability market growth to build enterprise clinical data strategies, incorporating specialized vendors with industry-leading technology to power all downstream functions. These solutions are designed to handle significant data volumes at incredible speeds, otherwise, impossible for human resources to manage.
Below we discuss how Availity Fusion is the best choice for health plans seeking to leverage clinical data and optimize ROI.
Accelerated Timelines
Standardized and Repeatable Outcomes
Significant Cost Savings
Alleviated Resource Burden
Scalability and Innovation

Availity Fusion’s API-based technology automates clinical data integration, normalization, and enrichment in real-time and at scale via a comprehensive five-step process known as Upcycling Data Availity Fusion supports multiple. business processes to drive significant financial, clinical, and operational improvements with an average processing speed that can upcycle an entire patient record in less than a second.
Proven on real-world data, Availity and its affiliated company’s depth of expertise, stems from dedication and focus on clinical data and industry data standards for nearly 10 years. The informatics clinical solutions team at Availity develops and maintains a proprietary data model to address poor data quality and clinical data complexities. The team comprises a diverse group of experts, including MDs, PharmDs, RNs, data scientists, terminologists, subject-matter experts, and business analysts who bring extensive industry and specialized experience. To ensure we maintain high data normalization uplift and stay aligned with industry specifications and regulations, the informatics team maintains a large terminology database with regular evaluation against real world data from leading organizations across markets. To date, Availity Fusion has processed clinical data from +160M patient lives and +640M clinical documents and this footprint continues to expand.
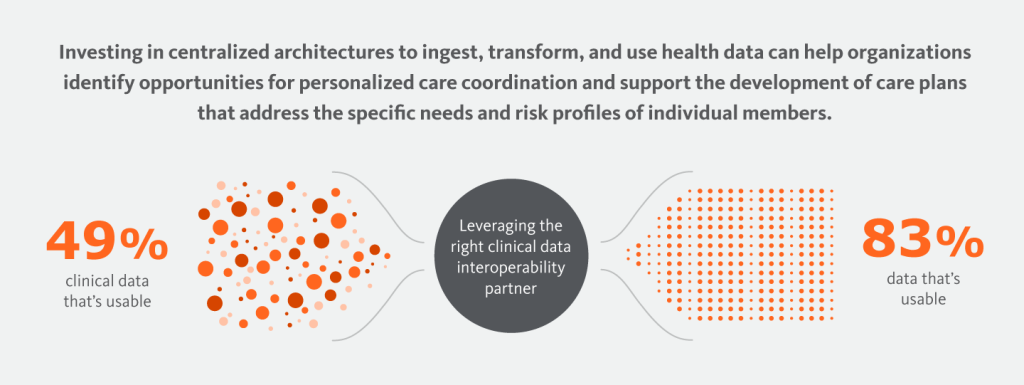
In a study performed across 14 distinct electronic medical record (EMR) systems and +500k clinical documents, Availity uplifted up to 83% of source data on average across 8 standard clinical domains, including medications, lab results, problems, and procedures.3
“To date, Availity Fusion has processed clinical data from +160M patient lives and +640M clinical documents and this footprint continues to expand.”
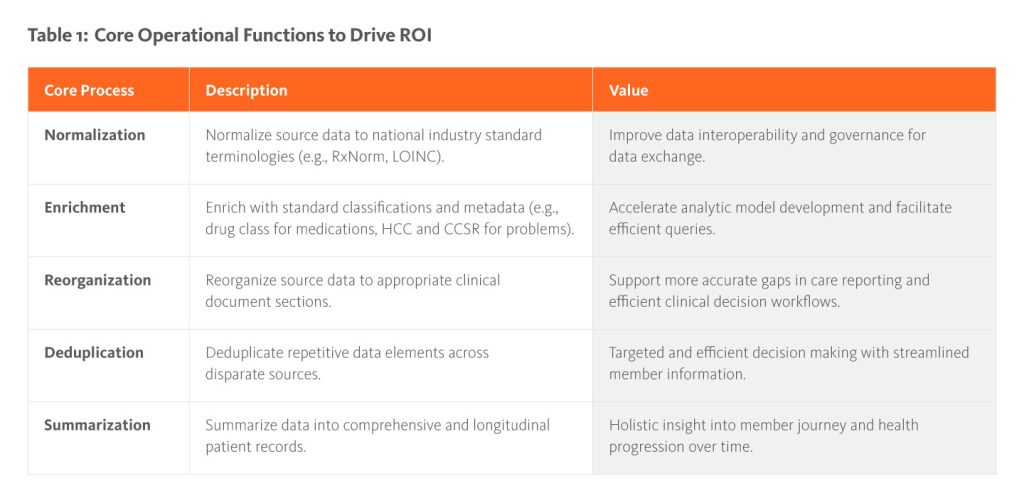
Availity Fusion offers a wide range of functionalities that automate complex and time-consuming data transformation tasks necessary to make clinical data useful across an enterprise. See Table 1: Core Operational Functions to Drive ROI for a comprehensive list.
Beyond the holistic approach to data quality improvement, bidirectional data conversion, and flexible enterprise integration, Availity Fusion offers industryleading speed and scale:
The following sections outline the impact of Availity Fusion’s speed, scale, and data quality improvement engine on health plan operations and cost.
Many organizations today operate with several, often siloed, data management functions happening concurrently. From the enterprise level, these parallel workflows are inefficient (sometimes duplicative), result in data inconsistency, and limit the reusability of the data downstream. In an example where risk adjustment, quality reporting, and clinical operations each perform components of data improvement independently, there are 3x the process, 3x the resources, and 3x the cost being borne by the plan. Availity is a critical part of an enterprise strategy, where a health plan wants to transform and store data once and use it across many use cases.
As described above, leveraging an automated, scalable technology to perform data quality improvement functions offers significant advantages compared to manual resources. To quantify the estimated cost savings associated with Availity Fusion’s automated technology, an Operational Cost Avoidance Model was developed. This model quantifies manual resource time and cost associated with core data enrichment activities. Additional efficiencies can be achieved when considering the work involved with integrating clinical data into architectural components, such as data lakes, and producing data fit for specific business purposes, such as for ingestion by a HEDIS® engine. These critical functions are not included in the model, which focused on core data enrichment.
“Additional efficiencies can be achieved when considering the work involved with integrating clinical data into architectural components, such as data lakes, and producing data fit for specific business purposes, such as for ingestion by a HEDIS® engine.”
Foundational principles of the model:
Availity Fusion inputs and assumptions used in development of the model are as follows:
Health plan inputs of the model are as follows:
Using these core inputs, the Operational Cost Avoidance Model is designed using the following calculation to generate total cost burden associated with investing in manual resources to perform data quality improvement:
A: Total manual resource hours per set of clinical documents
B: (A / # working hours per year per resource)
C: (B – # existing health plan resources)
D: (C * annual salary)
E: $ Net new hire cost burden
This analysis assumes manual data quality improvement across clinical documents in a 1-year period. As Availity Fusion’s technology improves data quality in sub-seconds per clinical document, this results in a significant efficiency factor for data quality improvement per source with Availity.
Finally, many organizations today operate with several data management functions happening concurrently, but in silos. In an example where risk adjustment, quality reporting, and clinical operations each perform components of data improvement independently, there are 3x the process, 3x the resources, and 3x the cost being borne by the plan. Additionally, this inhibits the sharing of best practices and creates inconsistent, poor outcomes from each siloed process. Shifting to an enterprise model with Availity’s platform used to inform all application of clinical data across business lines, health plans achieve additional efficiencies, cost savings, and optimal outcomes.

In partnership with a large, national health plan, Availity applied the Operational Cost Avoidance Model to determine total potential cost avoidance in a real-world example. This health plan invested millions in clinical data acquisition, but leveraging these assets in their raw, varied form resulted in incomplete and poor-quality measure performance, inaccurate risk adjustment reporting, and inefficient workflows across the enterprise. The health plan recognized the need to either build out a dedicated data enrichment function with new resources or leverage Availity’s technology for substantial administrative cost avoidance, accelerated data quality improvement, and enterprise integration.
Applying the Operational Cost Avoidance Model in partnership with this health plan across a subset of the member population, including 1.96M clinical documents and an average 2.62 clinical documents per member, Availity estimated up to $370M annually in anticipated cost avoidance. This represented the total amount of investment needed by the plan to hire and deploy new resources to process and improve a subset of their member data. With Availity Fusion, 100% of clinical data sources are optimized and 17,800x faster with its automated processes and consistent sub-second processing per Continuity of Care Document (CCD).
“With Availity Fusion, 100% of clinical data sources are optimized and 17,800x faster with its automated processes and consistent sub-second processing per Continuity of Care Document (CCD).”
The Operational Cost Avoidance Model demonstrates the ability for Availity Fusion’s technology to generate quantifiable cost avoidance and efficiency. It was also observed that, through use of this technology, data quality improvement processes are of higher quality and repeatable across business lines, existing resources can be strategically redeployed to accelerate innovation and advanced analytics, and enterprise businesses are more effectively positioned for future growth and scale of data operations.
Clinical data has gained significant attraction in the health plan market in recent years. However, in its raw form, clinical data is challenging to use and a strategic investment in data quality improvement and enterprise integration is needed to maximize value from data acquisition investments.
Leveraging manual processes to perform data improvement in silos
is inefficient, costly, error-prone, inconsistent, and not scalable.
Deploying an automated solution at the enterprise level is a
much better approach.
Availity Fusion provides automated functions for data preparation, enrichment, and enablement, resulting in considerable cost avoidance and efficiency gains for operations. This enables health plans to strategically reallocate their resources towards advanced analytics and innovation while reducing net new resource costs.
Availity demonstrated a potential cost avoidance of up to $370M annually for a large, national health plan and the ability to optimize clinical data 17,800x faster than manual resources.