Harnessing Data for a Healthier Future:
Overcoming Fragmentation to Improve Pandemic Response, Care Outcomes, and Equity
Overcoming Fragmentation to Improve Pandemic Response, Care Outcomes, and Equity
The COVID-19 pandemic has underscored the critical importance of sharing real-time data across the care continuum. However, despite the pressing need for accurate data, challenges persist in terms of data access, accuracy, interoperability, and silos among healthcare entities. These limitations significantly impede thorough analysis of crucial medical and demographic documentation, such as vaccination data and COVID-19 test results. As a result, healthcare organizations that lack a comprehensive understanding of the health status and needs of their populations are unable to effectively inform targeted public health interventions. This paper sets out to identify opportunities to address those challenges using semantic interoperability solutions to make the response to the next pandemic more streamlined, equitable, and evidence based.

The United States boasts one of the most technologically advanced healthcare ecosystems in the world. Unfortunately, optimal use of these advances has been blunted by a delivery system that is fraught with barriers and inefficiencies. Despite the volume and ubiquity of population and consumer health data, we are challenged with making this data accessible, interoperable, and usable.1 The U.S. spends more of its GDP on healthcare (17.1%) than any other developed nation, nearly double that of the next highest spender2 but cannot boast improved health outcomes. Some providers feel that this is due to a combination of factors, including challenges posed by lack of interoperability. We have an illness-based model of healthcare delivery, where reactive care for 50% of the population generates 86% of the total cost in the form of chronic illness management, end-of-life care, and acuity.3
Our ability to manage COVID-19, both from a prevention and a treatment of acuity standpoint, could have been an opportunity to shine, but it exposed some of these kinks in the armor even more so. While many harsh realities were brought to the forefront with the COVID-19 pandemic, we had experienced many of the same challenges, to a lesser degree with the H1N1 pandemic in 2009. These two recent experiences challenged state, local and federal government organizations and moreover, brought emergency departments and hospitals to their knees and impacted the resolve of medical providers on the front line. Throughout the pandemic, providers experienced shortage of diagnostic tests at testing centers to meet the population need and production and supply chain challenges with vaccines. Findings from an Association for Molecular Pathology survey found that more than 70% of U.S. clinical laboratories suffered significant delays related to COVID-19 testing programs.4 These delays were critical to the outcomes of individuals, communities, states and our nation with respect to the pandemic.
Healthcare professionals were challenged with identifying risk factors for severe disease and identifying impending death in those most sick. Sharing information on what treatments worked in different care settings across the nation evolved to this day, it has been a relative trickle compared to the possibilities afforded by the digital age. Healthcare systems failed to harness the power of multi-sourced, multi-formatted raw clinical data because of barriers imposed by standards of nonconformity, data siloes, and care fragmentation. As a result, providers found themselves rationing scarce medical resources to ensure that care for those in rural, urban, and suburban communities was delivered equitably.
During the H1N1 pandemic, Dr. Pinho was running an adult and pediatric medical practice in an upper middle-class neighborhood, which had been designated a state drop site for vaccinations and was fortunate to have received a surplus of vaccines for his patients’ needs. His colleague, an infectious disease doctor, was running a pediatric HIV practice in an urban teaching hospital and hadn’t received a single vaccine for a more at-risk population. The COVID-19 pandemic is studded with similar stories of social, racial and ethnic inequity. In this white paper, we identify three major challenges and opportunities for improvement in order to make future pandemic responses more efficient, fair, and based on solid evidence. The focus of this paper will be to explore how healthcare organizations can tackle challenges associated with data access and accuracy, overcome barriers to data interoperability, and integrate data silos to drive preventive measures, improve outcomes, and promote health equity. One of the most notable preventative tools in the healthcare system’s arsenal is the utilization of high-quality real-world data for efficient and effective decision-making.
“To effectively harness multisource and multiformat raw clinical data, healthcare organizations must first overcome challenges due to the lack of standardization, isolated data sources, fragmented care, and social, racial, and ethnic inequity.”
Vaccine equity is an important concern for racial and ethnic minority groups, as these groups have historically faced challenges with vaccine distribution and access. One of the major challenges with distribution is that many of these communities live in medically underserved areas. While predating the pandemic, the 2018 National Healthcare Quality and Disparities Report from the Agency for Healthcare Research and Quality (AHRQ), an HHS agency, confirms that non-Caucasian communities receive 40% worse healthcare across all measures.5 As a result, vaccine coverage is approximately 2.1 to 2.9 times higher for Caucasian populations relative to non-Caucasian populations, according to an issue brief by the Assistant Secretary for Planning and Evaluation (ASPE) Office of Science & Data Policy.6
As staggering as these numbers are, they likely do not reflect reality. Capturing and documenting race/ethnicity data has been a longstanding healthcare challenge. It is addressed later in this paper that a significant percentage of race and ethnicity goes undocumented. It is also addressed that minority populations are overrepresented in the cohorts of undocumented patients as compared to their non-minority counterparts. This poor data capture makes it difficult to fully understand who is getting vaccinated and who is not. According to the Kaiser Family Foundation’s report, data on COVID-19 vaccinations by race/ethnicity could be hindered by the inconsistent and non-interoperable documentation of these demographics across states and federal programs.7
“As a result, vaccine coverage is approximately 2.1 to 2.9 times higher for Caucasian populations relative to non-Caucasian populations”

Clinical data sourced from electronic health records (EHRs), labs, and health information exchanges (HIEs) contain unique and timely details on patients, such as vital signs, test results, diagnoses, immunizations, and more. However, the non-conformant coding, absence of key normalization, and poor data interoperability have obscured a real time, data-driven, longitudinal view of population health. Lack of interoperability has been particularly devastating for at-risk populations and data shows that infection, hospitalization, complications, and mortality varied significantly by race and ethnicity. This was exacerbated by poor data exchange between episodes of care.
Digital health technology is transforming the way we approach healthcare, and in particular, the adoption of systems to improve data quality and longitudinal health records has the potential to revolutionize patient care and health outcomes. Over the last two years, Availity has been collaborating with the California Department of Public health (CDPH) to identify and improve issues related to data quality, timeliness, and accuracy concerning public health reporting. Availity Fusion is our API, cloud-based technology engine that automates clinical data integration, normalization, and enrichment in real time and at scale through a comprehensive five-step process known as Upcycling Data.™
As part of that collaboration, our team of clinicians and informaticians performed an internal study on a yearlong cohort of 128 million lab reports that showed, among other findings, that race and ethnicity information was not documented in approximately 45% of cases. Through the implementation of the California Physician Reporting System (CPRS), this issue was addressed by identifying instances of poor data capture and returning to the original source for demographic data improvement.
“An internal study on a yearlong cohort of 128 million lab reports that showed that race and ethnicity information was not documented in approximately 45% of cases”
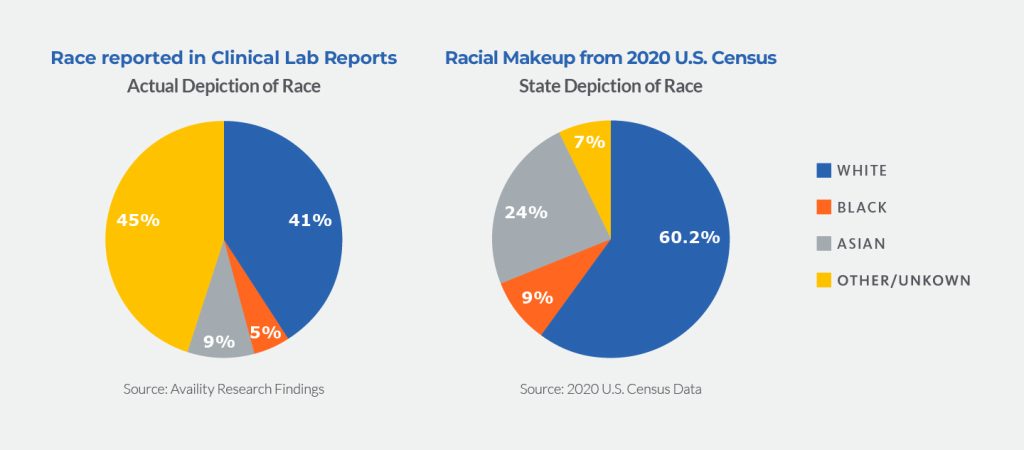
In the pie chart below, one can see that race and ethnicity are “other or unknown” in 45% as reported by laboratories. Census reporting of “other” race is 7%. Census reports of Caucasian race were 46% higher (41% of the population in the laboratory capture and 60% in census capture). As compared to Caucasians, Asians and Blacks are more likely to not have their race documented and are disproportionately represented in the “other or unknown” group. Their actual population numbers are 167% and 96% greater than those reported by labs.
Furthermore, our internal study identified that through outreach to source data providers an increase in the completeness of demographic information by 10% for all demographic variables and an estimated 25% across race and ethnicity categories was achieved. This study emphasized the importance of this information in the context of the COVID-19 pandemic, but also as a critical piece of any modernization strategy at the state or federal government level. Understanding the distribution of the disease across different populations is crucial for effective response and intervention.
While we have made progress in sub-categorizing data by demographic factors, such as race and ethnicity for the COVID-19 pandemic, it is important to also consider workstreams across other reportable diseases like influenza, RSV, and meningitis in order to gain a more comprehensive understanding of the population’s overall health status. Integrating comprehensive vaccination data with clinical documentation from medical providers, hospital settings, and self-testing for all patients is the necessary next step.
Quality data is the fuel that powers meaningful healthcare experiences and outcomes – now more than ever. We believe that an industry commitment to data interoperability standards and the application of technology to fix data quality will allow state and federal agencies to be better prepared to not only proactively monitor and address COVID-19 disease prevalence but also to strengthen our country’s public health reporting infrastructure more broadly. Data quality improvement can impact individual patient care and shepherd a data-driven response to not only the COVID-19 pandemic and future emerging pathogens but facilitate healthcare interoperability in general.
Availity has first-hand knowledge of the impact the wide variation in data quality had on the country’s response to COVID-19 from our work focused on cleansing, normalizing and enriching lab and clinical data for the government, data aggregators and other organizations. The reporting structure of diseases in many states is largely manual, with providers having to fill out PDF printouts and fax them to state officials so that they may be manually tallied and validated.
Lab reports for these diseases are also hampered by variability of coding and data incompleteness. In addition, vaccines administered for the COVID-19 pandemic were administered in public places by state and local officials and were variably entered in state vaccine registries. In order to complete their medical records, vaccinated individuals not only had to carry paper cards but also had to tell their medical providers their vaccine status. This worked somewhat well where there was continuity of care. However, in urban environments and other locations where continuity of care is unattainable due to various reasons, such as resource constraints, this is less likely to occur. Imagine a patient walking into an emergency department in florid shortness of breath, on the verge of intubation and in the absence of their family, having to relay vaccine status to complete their medical record. Treatment decisions were undoubtedly impacted, more so on those at the greatest risk. Data that could provide seamless care continuity for all and provide awareness and insight to care providers and public health officials was incredibly siloed.
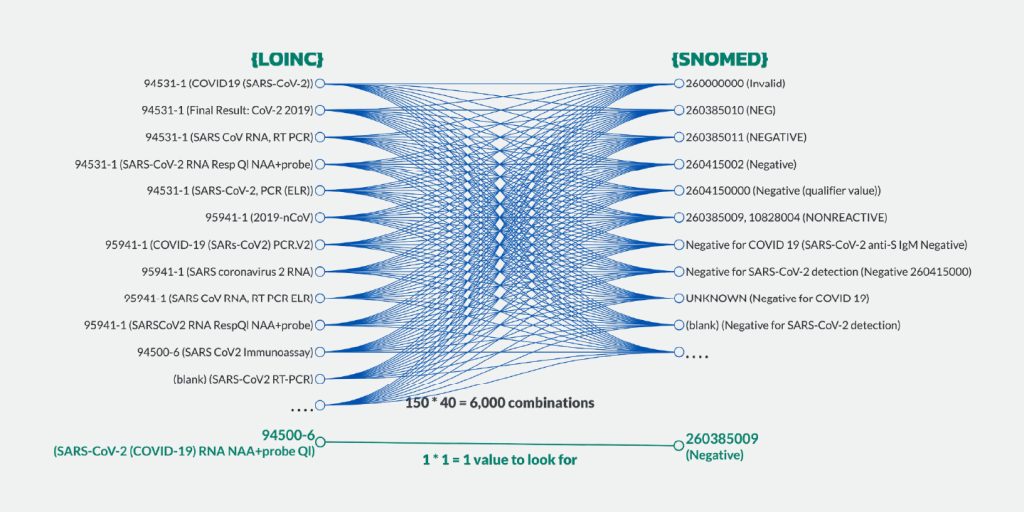
There are technological solutions for these persistent problems. During our ongoing work with Manifest MedEx to support the CDPH using Availity Fusion, we identified over 150 distinct variations of documentation of specific tests (e.g., the COVID-19 PCR test) and nearly 40 ways of documenting each negative or positive test result. As part of this collaboration, Availity Fusion’s API, cloud-based technology engine was used to analyze the quality of clinical data submitted, and automatically normalize it to the correct standards so that results could be quickly and accurately turned into appropriate actions aimed at limiting the spread of the disease. This included normalizing individual source variations in test type to a common Logical Observation Identifiers
“Using Availity Fusion, we identified over 150 distinct variations of documentation of specific tests (e.g., the COVID-19 PCR test) and nearly 40 ways of documenting each negative or positive test result”
Names and Codes (LOINC) and display name. Each variably documented source “positive” or “negative” was standardized to a common Systematized Nomenclature of Medicine (SNOMED) and display name. This uniformity enables downstream analytical capabilities to be more streamlined, intentional and actionable. As a result, while the quality of inbound data was found to be satisfactory in approximately 50% of cases, the outbound data quality achieved nearly 100% accuracy, completeness, and interoperability.
As depicted below, the representation of COVID-19 PCR test names was previously fragmented with 150 different display name and code combinations. Additionally, there were different SNOMED and display name combinations for positive and negative results. The implementation of a single LOINC standard code and display name for the same test, along with consistent display names and SNOMED codes for positive and negative results, has improved the standardization and interoperability of this information.
The ubiquity of self-administered home antigen tests made it difficult for state and federal agencies to capture and analyze results. Test numbers from outpatient and inpatient labs and wastewater analysis was largely the driver of these insights. The majority of at-home COVID-19 test results were not recorded in patient medical records. However, some at-home tests, such as the BD Veritor™ and the Lucira™ brands, allow for better reporting of results than simple patient interpretation by appending results to a valid LOINC code. This provides the opportunity for these at-home results to be recorded andshared in a standardized manner. While data-sharing and privacy issues will continue to be a perennial challenge, opportunities exist to help augment lab capabilities and public health data in times of increased need.
Pharmacies and states can partner with testing companies through state-level programs, allowing for direct access to results of tests performed by patients within a pharmacy setting or at home. The utilization of point-of-care tests featuring encoded standards that can be deployed in Fast Healthcare Interoperability Resources (FHIR®), in conjunction with the sharing of data via API enabled by the 21st Century Cures Act, facilitates the seamless transfer of information from patients to hospital systems, as well as between health plans and providers, thereby mitigating deficiencies in the continuity of care.
Solving for test result capture, both in the lab or at the point-of-care, is an important first step. Challenges around the limitations of paper-based vaccination records and cards also need to be addressed. One major issue is accessibility – paper records are often not easily accessible to healthcare providers, especially those outside the facility where the vaccinations were administered. Moreover, vaccine registries don’t always connect well to provider offices to relay results. As a practicing physician, Dr. Pinho describes a great information exchange with the vaccine registry. With respect to reciprocal receipt of data, those patients that received their flu shots at a pharmacy, while registry communication likely happened, there wasn’t seamless integration with his practice. Moreover, Dr. Pinho relates that his primary care doctor who is part of a large multispecialty group, did not receive information on his COVID-19 vaccination and relied on his report. Dr. Pinho’s current longitudinal record includes registry information for his county administered vaccine series and a duplicate entry of his self-report to his provider.
“The utilization of point-of-care tests featuring encoded standards that
can be deployed in Fast Healthcare Interoperability Resources (FHIR®), in conjunction with the sharing of data via API enabled by the 21st Century Cures Act, facilitates the seamless transfer of information from patients to hospital systems, as well as between health plans and providers, thereby mitigating deficiencies in the continuity of care”
One can see how this is a substantial data gap, making it difficult for providers to make informed decisions about patient care. Another issue is perpetuation of data – paper records can become lost, damaged or otherwise unreadable and patients can forget to self-report or dismiss it as irrelevant to their care. Beyond individual care impact it can ultimately influence the effectiveness of vaccination programs and the ability to track the spread of disease and its prevention in a timely fashion.
In contrast, the implementation of electronic transactions of data for vaccination records through FHIR resources has improved interoperability. States including, but not limited to, California, Kentucky, Massachusetts, and New Mexico that have rolled out “COVID-19 SMART Cards,” a digital record of a person’s COVID-19 vaccine history, are able to easily track and monitor the vaccination progress of their residents and share this information with providers and institutions. With the deployment of SMART Cards, nearly 500 million people globally now have digital access to their vaccine records.8 The integration of electronic transactions for the sharing of vaccine data among providers has the potential to enhance real-time data sharing as it pertains to this challenge.
The COVID-19 pandemic has emphasized the importance of enhanced interconnectedness and collaboration among all stakeholders in the healthcare system, such as providers, labs, hospitals, pharmacies, and registries, to ensure maximum benefits for the larger population. Through the electronic sharing of vaccine records we can accurately assess vaccination rates and investigate the connection between vaccines and breakthrough infections in the community. Furthermore, through the integration of provider data, it is possible to assess the probability of hospitalization and mortality in individuals who have tested positive for COVID-19 and have underlying health conditions, as well as measure vaccine efficacy. However, due to the scattered nature of existing data and difficulties with data quality, there are limitations in analyzing these relationships without a holistic solution that focuses on semantic interoperability and comprehensive data sharing.
“With the deployment of SMART Cards, nearly 500 million people globally now have digital access to their vaccine records”
Organizations across the healthcare industry are investing significantly in the acquisition and ingestion of many different sources of clinical data but are quickly realizing the journey to effective use has just begun. As depicted earlier, with multiple variations for representing positive and negative COVID-19 results, coding variations due to a lack of adherence to standards and inconsistent documentation in workflows creates an overwhelming amount of complexity. Health-related information sources, such as lab reports, provider visit notes, and hospital outcomes data are stored in various formats, including, but not limited to CVX, HL7v2 ORU, and CCD. This leads to an exchange of unstructured and inconsistent data.
Some organizations have tried addressing these issues using a variety of tools premised on mapping technology. Others have assigned data analysts and data scientists to tackle the complex framework of manually inferring missing codes such as core ingredient decomposition; allergy type classification (substance vs. food vs. medication); drug class; and reference ranges. These approaches are an unscalable and costly way to deal with data quality issues. At Availity, our customers and partners have transitioned from recognizing the potential of raw clinical data to having the power to deploy fit-for-purpose upcycled clinical data at scale.
“At Availity, our customers and partners have transitioned from recognizing the potential of raw clinical data to having the power to deploy fit-for-purpose upcycled clinical data at scale.”

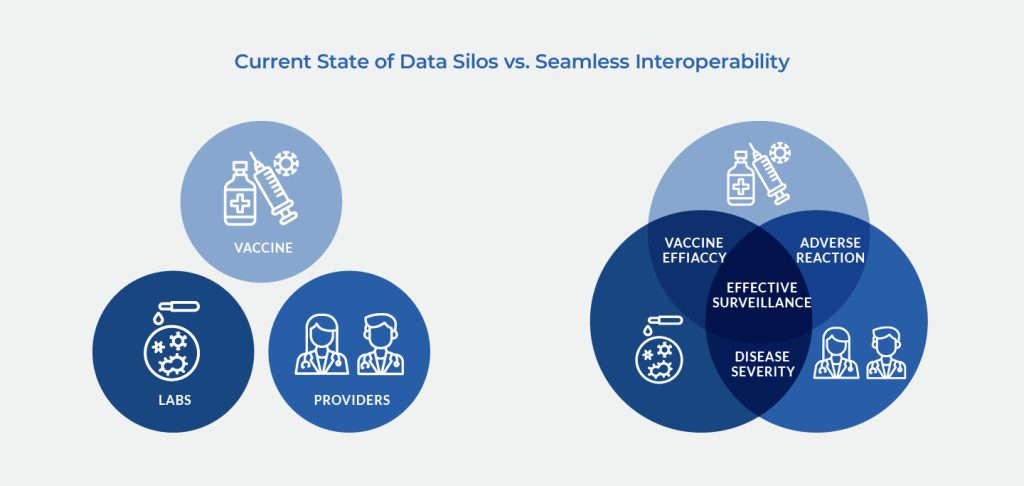
The healthcare industry has been grappling with multiple data silos, which have been a hindrance to effective data analysis and decision-making. With respect to the COVID-19 pandemic, three major sources of clinical data have largely been siloed: COVID-19 lab data, vaccination data, and provider encounter data. Data from these silos viewed in isolation only provides a limited understanding of one part of a patient’s health status and history. For example, COVID-19 lab data may only relay information on a patient’s positive or negative test result. How that information ties into vaccination status and ultimately outcomes, in the case of COVID-19 positivity is not discernable. Similarly, vaccine data might only offer details about the quantity and type of vaccines and booster shots a person has received, but it doesn’t capture positive test results or the severity of disease.
“Breaking down clinical data silos is essential for healthcare organizations to improve care coordination, reduce care gaps, and provide better patient care”
However, when these data silos are shared and integrated, they can paint a much more comprehensive picture of a patient’s health status and history. For example, if COVID-19 lab data is combined with vaccine data, healthcare providers can better understand the efficacy of the vaccines in preventing COVID-19. If provider data is also included, healthcare providers can gain a deeper understanding of the patient’s overall health status and develop more targeted and effective care plans when they do have positive tests. Breaking down clinical data silos is essential for healthcare organizations to improve care coordination, reduce care gaps, and provide better patient care. To achieve this, healthcare data consumers can start by investing in an integrated technology infrastructure that promotes seamless data sharing and interoperability. For public health, this infrastructure should facilitate the collection, analysis, and interoperability of high-quality data from various sources, including vaccine registries, labs, and provider-generated medical charts.

In addition to highlighting the need for semantic interoperability, this paper has also identified the crucial role that data quality plays in promoting health equity and completeness of accurate longitudinal health records. The impact of social drivers on health outcomes, such as health behaviors, education, community, socioeconomics, and the environment, is substantial. In communities that are most affected, data quality is hindered by various factors, including a lack of resources and time for physicians to address findings, inconsistent screening for health-related social needs, and difficulties with data collection.
Additionally, inconsistent primary and specialty care among socially disadvantaged individuals exacerbates the issue of poor data quality. To address these challenges and achieve health equity, it is important to improve data quality gaps. A semantically normalized record that is in line with national data quality standards and accessible across providers and care sites can help eliminate poor data quality that regretfully promotes inequities for marginalized communities. Addressing and improving data quality gaps is important to leveling the healthcare delivery playing field.
In conclusion, the COVID-19 pandemic has demonstrated the critical importance of real-time data acquisition, sharing and interoperability across the care continuum to enable effective and equitable healthcare delivery for all Americans. The challenges of data access and accuracy, interoperability, and silos within and between states and with the federal government have highlighted the need for semantic interoperability solutions that can bridge the gaps between disparate healthcare systems and data sources. By leveraging these solutions, healthcare organizations can gain a more comprehensive understanding of their populations, make more informed decisions regarding targeted public health interventions, as well as offer more prompt and pertinent treatment pathways. As the world continues to face new and evolving health challenges, high-quality data and semantic interoperability will play a vital role in ensuring that healthcare systems are equipped to respond effectively and equitably.
Availity Fusion is purpose built to take raw clinical data and use it to fuel emerging population health needs in a way that leads to quality experiences, outcomes and cost-effectiveness.
“As the world continues to face new and evolving health challenges, high-quality data and semantic interoperability will play a vital role in ensuring
that healthcare systems are equipped to respond effectively and equitably”