- Essentials Login
-
-
SolutionsBack
Solutions
-
For Payers
Simplify complex processes and improve payer-provider collaboration.
BackFor Payers
-
Payer Solutions Overview
Simplify complex processes and improve payer-provider collaboration.
-
Provider Engagement
Streamline workflows and improve engagement.
-
Provider Directories
Maintain compliance by capturing provider updates at the source.
-
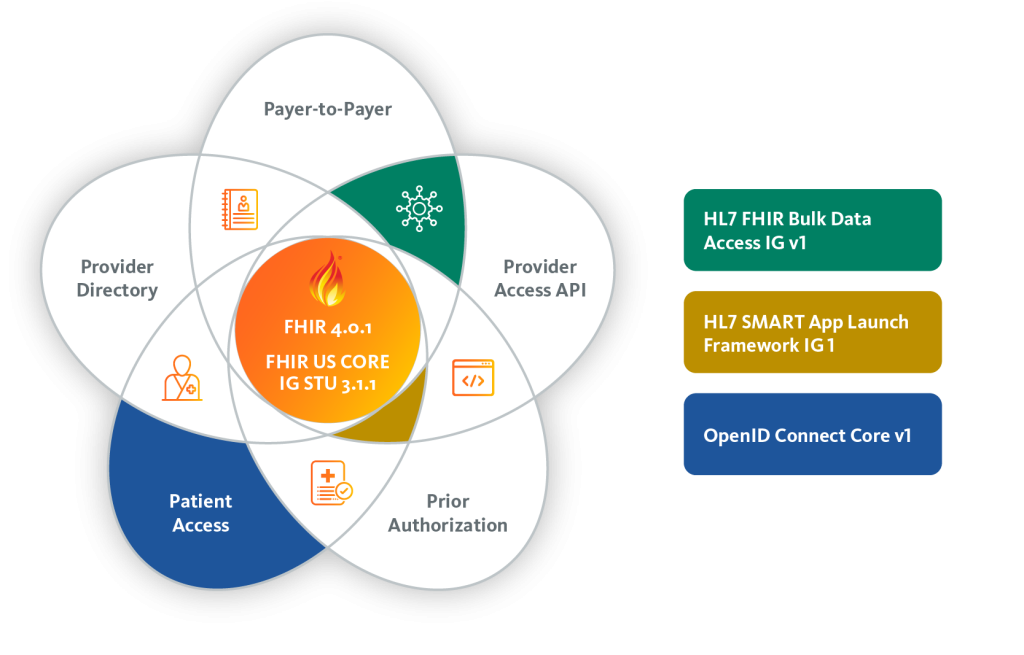
Interoperability
Transform data-sharing capabilities and reduce the cost of care.
-
End-to-End Authorizations
Ease prior authorization burdens with AI-driven solutions.
-
Digital Correspondence
Reduce print and postage costs and replace manual processes.
-
Payment Accuracy
Lower admin costs and prevent revenue leakage.
-
Payer Solutions Overview
-
For Providers
Streamline workflows, reduce denials, and ensure accurate payments.
BackFor Providers
-
Provider Solutions Overview
Streamline workflows, reduce denials, and ensure accurate payments.
- Revenue Cycle Management
-
Provider Solutions Overview
-
For Vendors
Seamlessly deliver complete and accurate healthcare information.
BackFor Vendors
-
Vendor Solutions Overview
Seamlessly deliver complete and accurate healthcare information.
-
Healthcare Connectivity
Facilitate seamless data exchange via X12, REST, and FHIR APIs.
-
Vendor Solutions Overview
-
For Payers
-
ProductsBack
Products
-
Multi-Payer Portal
Streamline provider workflows and improve collaboration.
-
Enhanced Payer Connectivity
Reach more health plans while streamlining pre-service and billing.
-
Revenue Cycle Management
Boost efficiency, prevent denials, expedite payments.
-
Clinical Data Transformation
Enhance clinical data quality for optimized downstream workflows.
-
Intelligent Utilization Management
Simplify the prior authorization review process.
-
EDI Clearinghouse
Connect to health plans nationwide.
-
Intelligent Gateway
Seamlessly connect and exchange administrative data.
-
API Marketplace
REST and FHIR-based APIs for fast, secure connectivity.
-
Provider Data Management
Maintain accurate provider directories.
-
Payer-to-Payer Hub
Streamline data exchange to meet mandatory compliance.
-
Multi-Payer Portal
-
InsightsBack
Insights
-
Case Studies
See success stories from our customers.
-
Blog
Get the latest industry insights.
-
Case Studies
-
ResourcesBack
Resources
-
Essentials Registration & Support
Get help registering or using Essentials.
-
Training & Education
Learn about our training courses.
- Essentials Payer List
- Essentials Pro Payer List
- Supported Systems
- Preferred Vendors
- Network Status
-
Essentials Registration & Support
-
About
-
ConnectBack
Connect
-
Contact Sales
Find the best way to get in touch.
-
Customer Support
Get in touch with customer support.
-
Locations
See where we're located.
-
Events
Learn about upcoming industry events.
-
Contact Sales
-